“When I was struck by the virus, within 24 hours I felt like I’d hit a brick wall,” says Zee. “Non-stop coughing, a fever spike… I was almost unresponsive – I could barely talk. It was terrifying.”
Zee was rushed in an ambulance to the Emergency Department at VGH and was quickly admitted into the ICU. With every hour that passed, his condition continued to deteriorate. Eventually, his breathing grew so weak that he was placed on a ventilator.
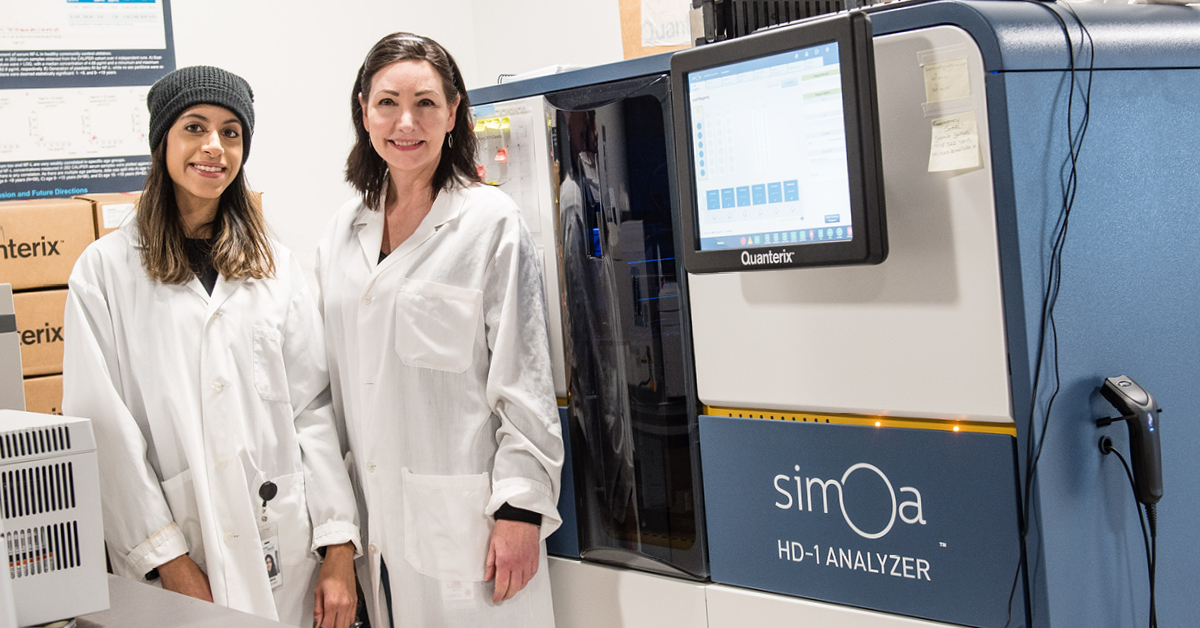
“I remember that moment so vividly – I truly didn’t know if I was going to make it,” says Zee. “Luckily for me, the doctors and medical experts at VGH are equipped with the latest knowledge, tools and technology. And through a clinical study led by Dr. Myp Sekhon (pictured above) and Cheryl Wellington, they saved my life.”